When their newborn patient’s heart is no bigger than a walnut, the one thing doctors don’t have room for is error. In a new collaboration between UW-Madison’s Department of Mechanical Engineering and School of Medicine and Public Health, Kuo K. and Cindy F. Wang Professor Tim Osswald, co-director of the Polymer Engineering Center; mechanical engineering graduate student Neil Doll; and joint Department of Mechanical Engineering and Department of Radiology Professor and cardiovascular modeling expert Alejandro Roldán-Alzate are using MRI scans and sophisticated 3-D printing technology to map and create patient-specific anatomical replicas.
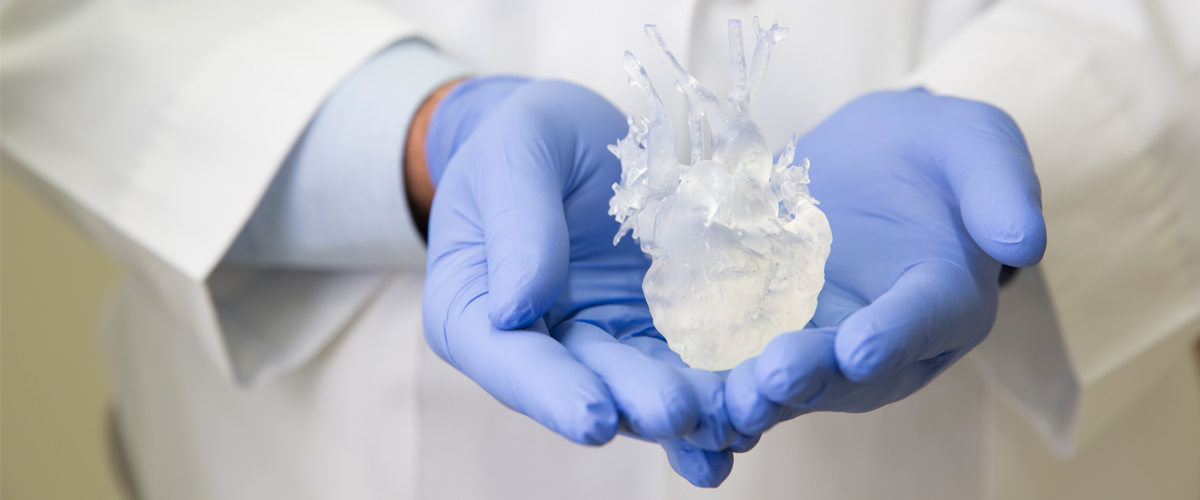
Children born with single ventricle heart defects—a condition in which the heart only has one functioning pumping chamber—often need to undergo a series of surgeries in the first years of life. Using a selective laser sintering (SLS) machine the size of a compact car, the team creates intricate, highly detailed models that accurately duplicate patients’ distinct heart defects.
The 3-D models can be connected to a pump that simulates circulation and then manipulated to mimic different conditions such as elevated heart rate—unlike a human cardiovascular system. Through these scenarios, engineers can help doctors observe exactly how a patient’s heart will beat and pump blood, without any risk to the patient’s health.
By running these in vitro experiments outside the body, surgeons can plan interventions for individual patients well before they make the first incision. This lessens the time a child spends in recovery—and even reduces the number of surgeries needed. Using 3-D printing to create patient-specific models helps doctors optimize surgeries to enhance blood flow, keeping the patient healthier for longer after a procedure.
